Standard Excision
Once the area is adequately numbed, the surgeon meticulously excises the lesion along with a small margin of healthy skin surrounding it. This margin is crucial as it helps ensure that all potentially abnormal or cancerous cells are removed, reducing the risk of recurrence. The excision is performed with precision to minimize scarring and promote optimal healing.
After the lesion is removed, the wound is carefully closed with sutures, which aid in the healing process and help achieve the best possible cosmetic outcome. Following the procedure, the excised tissue is typically sent to a laboratory for histopathological examination. This step is vital as it confirms whether all abnormal cells have been successfully removed and provides additional diagnostic information if needed.
At Lupton Dermatology, our surgeons specialize in performing standard excisions as a reliable treatment option for various skin conditions, including skin cancer. This procedure is an integral part of our comprehensive approach to skin health, ensuring that patients receive thorough and effective care.
By choosing a standard excision at Lupton Dermatology, patients can expect a high level of surgical expertise and personalized care. Our goal is to provide a safe and effective treatment that addresses the immediate concern and promotes long-term skin health. With a focus on precision and patient satisfaction, we strive to deliver the best possible outcomes, ensuring each patient feels confident and well-cared for throughout their treatment journey.
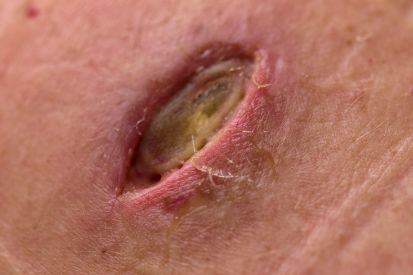
Examples of Standard Excision


Standard Excision Explained
Before the excision, patients typically undergo a consultation with the dermatologist, during which the need for the procedure is discussed, and any potential risks or benefits are explained. The dermatologist may recommend excision if a skin lesion raises concerns about malignancy, or if it causes discomfort or cosmetic issues.
Benefits of Standard Excision
How Lupton Dermatology in Greensboro, NC Can Help
Standard Excision FAQs
Your dermatologist might recommend a standard excision to remove a skin lesion or tumor for a few key reasons. Standard excision is often chosen for its effectiveness in completely removing malignant or potentially malignant growths, such as basal cell carcinoma, squamous cell carcinoma, or melanoma. This procedure allows for the comprehensive removal of the lesion along with a margin of surrounding healthy tissue to ensure that no cancerous cells remain, reducing the risk of recurrence. By excising a sufficient margin of normal tissue, your dermatologist can also conduct a thorough histological examination to confirm that the margins are clear of cancerous cells, providing a more definitive treatment outcome.
Additionally, standard excision might be recommended for certain benign but problematic lesions that could pose future health risks or cosmetic concerns, such as large moles, cysts, or lipomas. This method not only removes the visible lesion but also addresses any underlying tissue involvement, leading to better cosmetic results and minimizing the chances of the lesion regrowing. The procedure is straightforward and typically performed under local anesthesia, making it a practical option for both the patient and the dermatologist.
No, a standard excision is not painful. Your dermatologist will use local anesthesia to ensure the area is completely numb before the procedure begins. This anesthesia effectively blocks any sensation in the treated area, allowing the procedure to be performed without causing pain.
What to Expect During the Procedure:
Administration of Anesthesia:
- Local Anesthesia: A numbing agent is injected into the skin around the lesion. This process may cause a brief stinging sensation, but it quickly takes effect, numbing the area completely.
- Comfort Maintenance: The dermatologist will ensure you are comfortable and the area is fully anesthetized before proceeding with the excision.
During the Excision:
- Sensation of Pressure: While you will not feel pain, you may experience some pressure or a tugging sensation as the dermatologist removes the lesion. This is normal and should not be uncomfortable.
- Focused Care: The procedure is carried out with precision to minimize discomfort and achieve the best possible outcome.
Post-Procedure Sensations:
- Mild Discomfort: After the anesthesia wears off, you might experience mild discomfort or soreness at the excision site. This is typically manageable with over-the-counter pain relievers.
- Healing Process: Your dermatologist will provide detailed post-operative care instructions to manage any discomfort and ensure proper healing.
Ensuring a Pain-Free Experience:
- Pre-Procedure Consultation: Your dermatologist will discuss the procedure with you in detail, addressing any concerns you may have about pain management.
- Ongoing Support: Throughout the procedure, the medical team will monitor your comfort levels and make adjustments as needed to ensure a pain-free experience.
A standard excision procedure is generally quick and efficient. The duration of the procedure primarily depends on the size and location of the lesion, as well as the complexity of the required closure. On average, a standard excision can be completed within 30 minutes to an hour.
After a standard excision, the removed tissue is typically sent to a pathology laboratory for histopathological examination. This process involves a pathologist examining the tissue under a microscope to determine the exact nature of the lesion. For suspected cancerous lesions, this analysis is crucial to confirm whether the growth is malignant or benign. The pathologist will also assess the margins of the excised tissue to ensure that all cancerous cells have been removed. Clear margins indicate that no cancer cells are present at the edges of the removed tissue, suggesting that the excision was successful in removing the entire lesion.
The results from the pathology report help guide further treatment decisions. If the margins are not clear, indicating that cancerous cells may remain in the body, the dermatologist may recommend additional surgery or other treatments, such as radiation or chemotherapy. Conversely, if the pathology report confirms benign or adequately excised tissue with clear margins, no further treatment may be necessary beyond routine follow-up. This step is essential for accurate diagnosis, effective treatment planning, and ensuring the best possible outcome for the patient.
Yes, there will likely be some scarring after a standard excision, as it involves making an incision in the skin to remove the lesion and then closing the wound with sutures. The extent and appearance of the scar depend on various factors, including the size and depth of the excised lesion, the location on the body, the patient’s skin type and healing ability, and how well post-procedure care instructions are followed. Generally, dermatologists aim to minimize scarring by making precise incisions and using appropriate suturing techniques. Over time, scars typically fade and become less noticeable, though they may not disappear entirely.
Proper wound care is essential for reducing scarring. This includes keeping the wound clean and moist, following the dermatologist's instructions on bandaging, and avoiding activities that might stress the wound. Additionally, the use of silicone gels or sheets, scar creams, and sun protection can further help in managing the appearance of the scar. In some cases, if the scar is particularly prominent or bothersome, treatments such as laser therapy, steroid injections, or surgical revision can be considered to improve its appearance. Overall, while some scarring is inevitable, its impact can be significantly mitigated with proper care and treatment.
Yes, there are several alternatives to standard excision for treating various skin conditions, depending on the specific diagnosis, size, and location of the lesion, as well as patient preferences and overall health. One common alternative is Mohs surgery, which is particularly effective for skin cancers like basal cell carcinoma and squamous cell carcinoma. Mohs surgery involves the precise removal of skin cancer layer by layer, examining each layer under a microscope until all cancerous cells are removed. This technique spares as much healthy tissue as possible and offers high cure rates, making it ideal for lesions in cosmetically sensitive areas.
Other alternatives include cryotherapy, which involves freezing the lesion with liquid nitrogen, and electrosurgery, which uses electric currents to burn and destroy abnormal tissue. Laser therapy can also be used for certain skin conditions, offering a non-invasive option that uses focused light to remove or reduce lesions. For benign lesions like warts or skin tags, topical treatments or chemical peels might be recommended. Each alternative comes with its own set of advantages and potential drawbacks, and the best choice depends on individual factors such as the type of skin condition, its location, and the patient's medical history. Consulting with a dermatologist is essential to determine the most appropriate and effective treatment option.
What to Expect at Your Standard Excision Appointment
Post-excision, the dermatologist closes the wound using sutures or other methods based on size and location, providing patients with post-operative care instructions, including wound cleanliness and activity restrictions during healing.
How to Prepare for Standard Excision
Planning for Standard Excision Recovery
We will work with you to ensure proper recovery and are happy to answer any questions you have.
Featured Products
Check your local office for current stock!
Check your local office for current stock!
